Blog
All blog posts ordered by publication date

26 April 2024
New blueprint for locally led growth
A new co-creative approach from national innovation programme could set a new blueprint for locally led growth.
23 April 2024
Shakespeare’s language: a voyage through numbers
How a new approach to analysing Shakespeare’s language has revolutionised our understanding of what he wrote and placed it in the context of other writers.

18 April 2024
Smart grants: catalysing high impact innovation and market share
Smart grants support and propel groundbreaking, world class projects from UK business designed for commercial success, market impact and UK economic growth.

18 April 2024
Activating communities for regional renewal
Research and innovation are crucial to delivering benefits across the UK. But how can we achieve this while appreciating the unique needs of specific areas?
10 April 2024
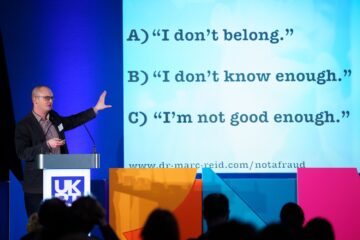
Compare carefully to manage your inner imposter
We invite Marc Reid, UK Research and Innovation (UKRI) fellow, to discuss how we can better manage the moments in which we compare ourselves to others.





